Keratoconus can develop subtly and gradually, so it is important to stay on top of your regularly scheduled eye examinations to prevent potential degradation of your vision. In less severe cases, specialty lenses and therapy can be used to mitigate the effects of keratoconus, but if the issue is an advanced case, surgery or a cornea transplant may be necessary.
What is Keratoconus?
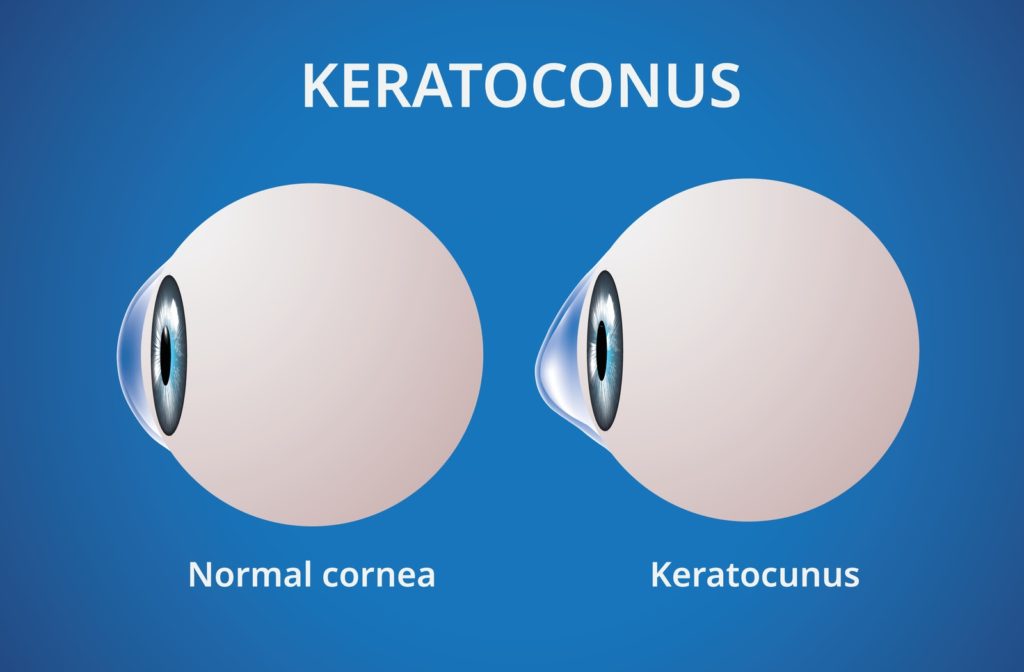
Keratoconus is when your cornea (the clear, dome-shaped front surface of your eye) thins and gradually bulges outward into a cone shape. This can cause blurred vision and increased sensitivity to light. Keratoconus usually occurs in both eyes and can affect each of them to different degrees. Keratoconus generally begins to affect people between the ages of 10 and 25.
Preventing Keratoconus
If caught in its early stages, you can potentially treat keratoconus through the use of glasses or soft contact lenses. Later on, if you are still experiencing symptoms of keratoconus, you may have to be fitted with rigid, gas-permeable contact lenses or other types of lenses, such as scleral lenses. If these methods do not help in treating your condition, you may need a cornea transplant.
Symptoms
Some symptoms of Keratoconus are:
- Blurred or distorted vision
- Increased sensitivity to bright light and glare, which can cause problems with night driving
- A need for frequent changes in eyeglass prescriptions
- Sudden worsening or clouding of vision
Causes
Currently, the cause of Keratoconus is unknown, although genetic and environmental factors could contribute to developing the condition. Around 1 in 10 people with keratoconus also have a parent with the condition.
Complications
- Your cornea may swell in some cases. This can potentially cause reduced vision and scarring. This swelling is caused by a condition in which the inside lining of your cornea breaks down, allowing fluid to enter the cornea.
- Advanced keratoconus may cause your cornea to become scarred where the cone is most prominent.
Treatment Options for Keratoconus
Different treatment options are available depending on the severity of your condition. Mild to moderate cases of keratoconus may only require corrective eyeglass or contact lenses, while more advanced cases may necessitate surgery or a cornea transplant.
Lenses
- Eyeglasses or soft contact lenses can correct blurry or distorted vision in early keratoconus. Although, as the shape of your cornea changes, you will frequently need to change their prescription for eyeglasses or contacts.
- Hard (rigid, gas permeable) contact lenses are usually the next step in treating keratoconus. This type of lens can be made to fit your corneas.
- Piggyback lenses – If just wearing rigid lenses on their own are uncomfortable for you, your doctor may recommend “piggybacking” a hard contact lens on top of a soft one.
- Hybrid lenses have a rigid center with a softer ring around the outside for increased comfort and can be a good option for those who find rigid contact lenses uncomfortable.
- Scleral lenses are useful for very irregular shape changes in your cornea in advanced keratoconus. Scleral lenses sit on the white part of the eye (sclera) without touching the cornea.
Therapies
- Corneal collagen cross-linking – In this procedure, the cornea is saturated with riboflavin eye drops and treated with ultraviolet light. This causes the cornea to stiffen, preventing further shape changes. Corneal collagen cross-linking may help to reduce the risk of progressive vision loss by stabilizing the cornea early in the disease as a preventative measure. Some of the benefits of corneal collagen cross-linking include:
Surgeries
Some surgical options to treat keratoconus include:
- Penetrating keratoplasty – A cornea transplant procedure may be necessary if you have corneal scarring or extreme thinning. In this procedure, doctors remove a full-thickness portion of your central cornea and replace it with donor tissue.
- Deep anterior lamellar keratoplasty (DALK) – This procedure preserves the inside lining of the cornea (endothelium). This helps avoid the rejection of this critical inside lining that can occur with a full-thickness transplant like a penetrating keratoplasty procedure.




